Kansas has invalidated, overnight, the driver’s licenses of transgender people who changed their stated genders to match their identities. This apparently affects about a thousand people in the state, with no grace period, as of three days ago. “The law also prohibits transgender people from using multi-occupancy bathrooms in government buildings that do not correspond to their sex assigned at birth, and authorizes private citizens to sue people who violate the law.” —Reuters
According to three academic researchers writing for The Conversation, a media source rated ‘Least Biased’ and ‘Very Highly Factual’ by Media Bias/Fact Check:
“Roughly a quarter of trans and nonbinary people who have not updated their identification documents experience subsequent mistreatment when showing their IDs, including verbal harassment, assault and denial of services or access to settings. In our research, we similarly found that not having one’s gender legally affirmed is associated with greater discrimination and social rejection – one pathway to negative effects on mental and physical health.
“To comply with the current law sets up an impossible situation for many trans and nonbinary people who have been using the restroom aligning with their gender identity and presentation for years. These individuals are set up to face violence, legal action or criminal penalties even when they are complying with the law, as using the restroom aligned with their sex assigned at birth will appear to others as contradicting their gender presentation.”
The US House of Representatives has passed the SAVE Act, which will “require everyone registering to vote to provide a document verifying their citizenship and implement strict photo ID requirements to vote.” —The National Conference of State Legislatures
Nine Things to Know about the SAVE Act from the NCSL:
- Federal law is clear that only U.S. citizens are permitted to vote in federal and state elections. Currently, states decide how to enforce this requirement. All states require new voters to attest to their U.S. citizenship when they register, and all states conduct voter list maintenance to identify potentially ineligible voters on the rolls. How they do that varies.
- The SAVE America Act would require states to collect and document proof of citizenship from voters, which few states currently do, and establish additional voter list maintenance processes. A recent University of Maryland study indicates that as many as 21 million eligible voters do not have easy access to documents proving citizenship.
- The bill would implement a strict photo ID requirement for federal elections and specify the types of identification accepted. While 36 states currently have voter ID requirements to vote, state approaches vary. Just 10 states fall into the strict photo ID category, as defined by NCSL.
- The bill’s identification requirements also specify that a voter ID document must indicate that the individual identified is a U.S. citizen. A handful of states denote citizenship status directly on driver’s licenses, and while applicants for REAL ID cards provide documentary evidence of citizenship status, the cards display the same gold star insignia for a citizen as for a lawfully present noncitizen. Currently, each state determines the types of ID acceptable to vote, and that often includes student IDs, hunting and fishing licenses or other state-specific identification cards.
- The bill would require voters registering to vote by mail to submit documentary proof of citizenship, which states do not currently require. It is unclear how the bill would affect online voter registration, which is an option in 42 states.
- The bill would require voters applying for and submitting absentee/mail ballots to submit a photocopy of their identification, at both steps in the process, which most states do not currently do.
- The bill does not authorize federal funding for the new state responsibilities it creates, and it includes no phase-in period.
- States that can’t comply might face running state and federal elections separately, with separate procedures, or they might have to keep separate lists of voters who have not provided proof of citizenship and permit them to vote only in state or local races. Arizona already has such a “bifurcated” process, which has seen a stream of litigation dating to 2004.
- The bill would require states to run their voter lists through the Systematic Alien Verification of Eligibility system to identify potential noncitizens on the voter rolls. Many, though not all, states use this system as one resource for identifying potential noncitizens, but not at the frequency this bill envisions. There are also questions about the personal voter information states would be asked to provide to run records through the database.
The bill also includes a private right of action, allowing individuals to sue if they feel the law is not properly enforced. It would establish criminal penalties for election officials who mistakenly register an applicant to vote who has not presented proof of citizenship.
To learn more about state actions, see the State Legislatures News story “States Consider Options to Ensure That Noncitizens Aren’t Voting” and NCSL’s webpage Legislative Approaches to Ensuring Only Citizens Vote.
House Resolution 7661, the Stop the Sexualization of Children Act, was introduced by Illinois representative Mary Miller and 17 Republican cosponsors on February 24. “The legislation amends Section 8526 of the Elementary and Secondary Education Act of 1965 to prohibit federal funds from supporting any school programs, activities, literature, or materials for minors under 18 that include ‘sexually oriented material.’ It explicitly defines ‘sexually oriented material” to encompass content involving “gender dysphoria or transgenderism,’ alongside depictions of sexually explicit conduct such as nudity or lewd dancing.” —The Edge Media Network:
“LGBTQ+ advocates have raised alarms about the bill’s implications for transgender students and educators. It could compel transgender teachers to conceal their identities and deter schools from affirming transgender students’ identities due to fears of losing federal funding. The vague wording might effectively erase transgender visibility in public education, impacting mental health resources and inclusive environments for transgender youth… H.R. 7661 represents a significant escalation by tying transgender topics to federal education funding, potentially affecting schools nationwide if passed. As of February 26, 2026, it remains in committee with no further action reported. LGBTQ+ groups continue to monitor its progress, emphasizing the need for inclusive educational spaces for transgender people.”
From the American Library Association:
“In response to H.R. 7661, introduced on February 24, American Library Association President Sam Helmick issued the following statement:
‘Parents, not politicians, should guide their children’s reading. In our school, campus, and public libraries, materials are selected by trained literacy professionals who understand child development and community needs. Their work is grounded in one clear purpose: helping young people become lifelong readers.
‘H.R. 7661 isn’t fundamentally about protecting kids. It’s about giving politicians broad authority to restrict whose stories are allowed on our shelves. That should concern anyone who believes in the freedom to read and the right of families to make decisions for themselves.
‘Rather than targeting librarians and teachers, Congress should invest in them. The Right to Read Act offers a better path, supporting well-staffed and well-resourced school libraries, strengthening evidence-based literacy instruction, and protecting the dedicated professionals who help young people discover books that open doors and expand horizons. When we trust families, support educators, and protect the freedom to read, our young people thrive.’”
I feel alarmed, my friends. Never before have I felt this urgent and anxious about impending (and, frankly, in progress) federal action or legislation that directly disrupts the lives of so many people. My social media feed paints the worst case scenario for all of the items above, and the severe alarm is not unjustified, no matter what my conservative friends may say. Looking at implementation, enforcement, and consequences for violation of sweeping, vaguely worded laws that allow no time for thoughtful, local execution, I am especially worried about effects of the SAVE Act on the midterm elections this year. I want my Red voting friends to acknowledge the possibility of harm done to vulnerable populations and excluding them from exercising their right to vote, thereby skewing election results toward the right.
I ruminated about this post all day and procrastinated most of this evening to write it, feeling agitated and ambivalent. What do I want from my friends in the wake of all this distress?
Two Blue voting friends expressed hopelessness to me this week. “It’s going to come down to rioting in the streets,” said one. “There is no more compromising left,” said the other. Both do not see a path forward for civil political discourse in any form. “I will not talk to the guy dragging people out of their cars at gunpoint,” and “…there is not dialogue that is possible until the far right starts to feel the consequences of this regime.” What struck me about these expressions was their focus on the extreme. I don’t seek engagement with ICE or border patrol officers actively engaged in detaining civilians on the street, and I don’t generally encounter far right political extremists. I still hold that political discourse is not only possible but more necessary than ever, if we are to save our country from accelerating, exponential, adversarial political escalation and even violence. And it has to occur between and among us regular folks.
When I think about my Red voting friends, however, I can easily imagine any and all of my progressive concerns being dismissed out of hand. “Just show your birth certificate or passport, no big deal,” they may say. How many of us have our birth certificates readily available? If not, how easy would they be to obtain? About half of US citizens do not hold a valid passport. What about people (mostly women) whose names changed when they got married? Who still has their marriage certificate ready to present? It’s the extra hassle and inaccessibility/inability to comply with all these rules that we Blues worry will disenfranchise otherwise legitimate voters. That has consequences, which many on the left believe is the goal of those on the right.
I hesitate to include quotes here discussing the worst case scenarios precisely because I anticipate the most likely response from conservatives to be flat out rejection and invalidation of my concerns. That kind of response shuts down engagement and exchange, and I want no part in inciting it. I realize only as I write this now, that this is the greatest barrier to my expressing anything emphatic or alarming to my conservative friends. For over a decade now my fears and worries have been consistently minimized and discarded as catastrophizing and hysterical, essentially. I have never been asked why I feel fear, or what evidence there is to justify it. Examples I raise are almost always discarded as ‘fake news’ in one way or another. My concerns are not acknowledged as valid, much less empathized with. It feels disrespectful, condescending, thoughtless, and degrading, actually.
There’s not much effective political advocacy I can do locally. Both of my senators and my representative are Democrats and will vote against the legislation that I oppose. I will likely never live in a district where my vote may swing an election (very few of us do). So where does my agency lie? I think we need to elevate and elect candidates willing to listen to their opponents more generously than most elected officials do now–on both sides. We need leaders with both the skills and willingness to treat opposing ideas and people who hold them with humility and respect rather than contempt and dehumanization. We especially need to get the chief dehumanizer and his unqualified staff out of the highest office in the land, to restore decency and government for the people at the very top.
But how can we elect reasonable, decent, level-headed political leaders if we, the voting citizenry, refuse to engage each other with the same attitude of mutual respect and human decency? What will it take to stop generalizing ‘all Democrats’ and ‘all Republicans’ into mental trash bins only to be spat on and dumped in rhetorical landfills? I wrote to my Blue voting friend tonight, “Compromise may not be the right word or concept, but we must stay at the table to engage and negotiate. There will be no ‘vanquishing the enemy.’ There is no winning in the sense that everyone wants. We must find a way forward together with everyone. We have to all participate in the de-escalation.”
There is a kernel of truth in every reasonable assertion on every side of an issue. Our job as participants in civil discourse, in service of de-escalation and finding a collaborative path toward our shared goals, is to seek and acknowledge these kernels in our opponents’ arguments, and use them to sharpen our own. There are people who do this well, like Mónica Guzman; we must seek and amplify their voices.
One example is the Substack article “You’re Probably Wrong About the Deportations” by Jonathan Stray, writing for the Better Conflict Bulletin. I quote large exerpts here to make the point about seeking and highlighting nuance and partial, incomplete truths in our daily discourse, guarding against superfluous, overgeneralized, oversimplified, and derisive language and assertions:
“Which of these stories about immigration do you believe?
- “Many millions of unauthorized immigrants had been living happily as contributing members of American communities for decades, until ICE started cruelly and violently arresting them under the Trump administration.
- “The Democrats let untold millions of violent criminals into our country. ICE is merely enforcing existing laws to remove murderers and rapists, a long over-due increase in deportations.
“As is so often the case, these conflicting stories are both partially right. Because of the intense polarization on this topic, most people believe an uncomfortable mix of truth and half-truth.
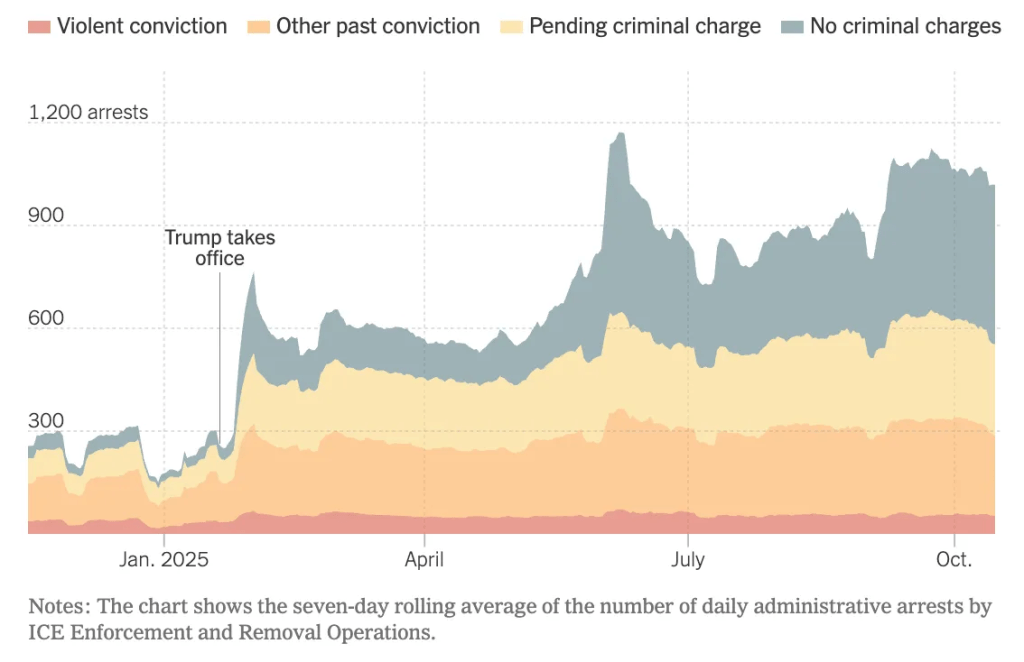
“Red frame problems: The ‘enforcing existing law against criminals’ frame is contradicted by the administration’s own data and its own officials’ statements. They’re not primarily deporting criminals; they’ve eliminated criminal prioritization, set arrest quotas, and 73% of detainees have no convictions. ‘Border Czar’ Homan says non-criminals will ‘go too.’ MAGA voices like the Heritage foundation criticize the administration for not deporting all unauthorized immigrants.
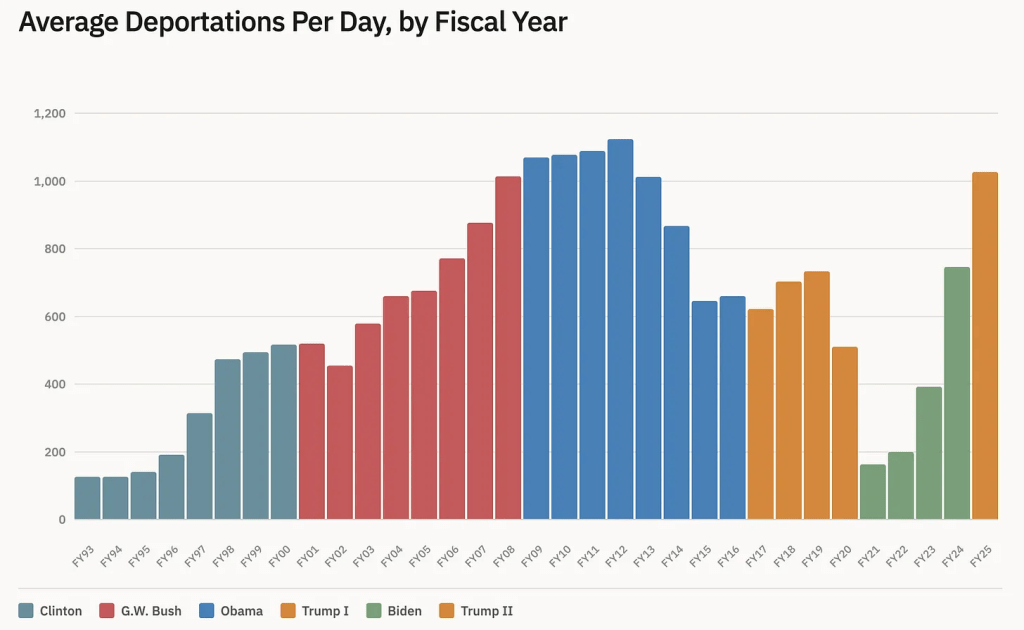
“Blue frame problems: The ‘happy contributing members living peacefully for decades’ frame misses that there genuinely was a massive increase in unauthorized immigration under Biden (from 458,000 in 2020 to a record 2.2 million in 2022), that this caused enormous stress on some communities, that there are more than a million unexecuted removal orders from immigration judges, and that the Obama administration was itself deporting ~1,000 people per day in its first term, about the same as Trump is currently managing.
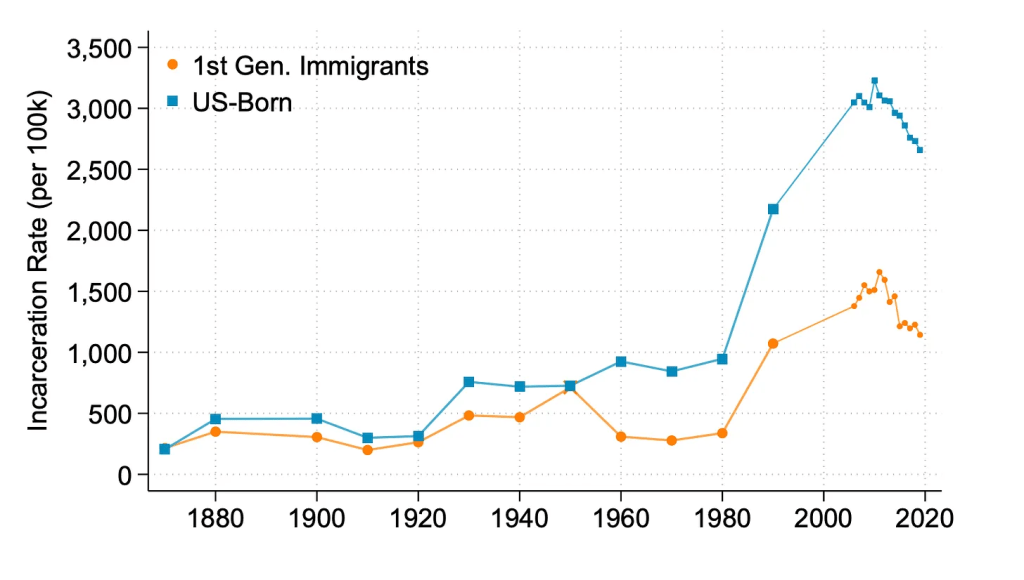
“The overwhelming majority of immigrants (of whatever kind) are law abiding. Every possible statistic on the topic shows this clearly. Only 23 out of 14,500 homicides in 2025 were by unauthorized immigrants, according to CBP. Overall, immigrants (of whatever kind) commit fewer crimes than U.S. born citizens, and have for the last 150 years.”
“Most Red Americans believe that the Trump administration is deporting only people with a criminal record, while most Blue Americans believe the opposite. Both are half right. A majority of those arrested so far have a criminal record. But the share of arrests of people without a criminal record are increasing.”
“Part of what is going on here is that a vocal Red minority want to restrict immigration generally, unauthorized or not. The Administration’s public message has mostly been about removing unauthorized immigrants with a criminal record — and this idea remains very popular. Yet the underlying legal instruments do not make this distinction, and many Administration officials have repeatedly said the goal is to remove all unauthorized immigrants — a policy which is unpopular among Americans generally.
“So there is a political bait and switch happening here: the Administration is saying that it’s all about criminals, as with their slick “worst of the worst” site. But a bit over half of Republican voters want all unauthorized immigrants gone, and in fact arrests are increasingly shifting to people with no criminal record.
“If it feels like we’re in a new era of immigration enforcement, we are. But this isn’t really because more people are being deported. Rather, the focus has shifted to interior enforcement in cities, which is more likely to target people who have been here for some time.
“On top of this, Trump is targeting ‘Democrat’ cities and states (in his own words) which is about political “retribution” (in his own words). This of course feels deeply unfair to Blue America.
“Hopefully, you learned something in all of this. There’s an argument over whether the Administration is really deporting just “the worst of the worst” as they repeatedly claim. Is ICE deporting murderers and rapists? Yes, but mostly no. There’s an argument over whether deportations are even up at all. Do we live in an era of mass deportations? Not more so than under Obama, but the who and where has drastically changed.
“With any luck, this dive into into the weeds of immigration enforcement will help you have a better conversation the next time you get into it with your misguided relatives. If we’re fighting, at least we should be clear on what we’re fighting about.”
It took hours to search, curate, and quote all of the articles included here, and I’m glad I did it. It showed me that I am justified in my grave concerns for governmental overreach and its severe negative potential consequences for many people. It also showed me that actively and methodically vetting the most emotionally inciting claims almost always de-escalates my psyche and restores my sense of agency to engage with reason and equanimity.
Connection and persuasion felt opposed when I first conceived of this post. Now I reaffirm that the latter cannot occur without the former, of course. And my persuasion goals now center around shared principles and finding better, more moderate methods for expressing them, more than debating specific legislation. That doesn’t mean I will shy away from discussing risks and harms I see specific policies presenting, but I will do so still from a perspective of curiosity, mutual respect, and seeking a collaborative rather than oppositional path forward.
I’m still alarmed. More and more policies, both in proposition and execution, feel extreme, dysfunctional, and harmful for too many–far more than just the few I highlight here. I’m also still convinced and committed that we regular folks, when we exercise our responsibility to engage in conscientious media consumption, respectful civic discourse, and holding our leaders to the same standard, can ebb the tide of escalating adversarial politics.
I am not hopeless. I am energized and impatient, and I intend to continue to channel this powerful humane force toward connection above all else. Because connection is the foundation of all movement that matters.